.jpg)
Ensuring accessible and affordable healthcare is a cornerstone of any thriving society. However, worldwide healthcare expenditures continue to escalate at an unsustainable rate, straining public finances and leaving millions without adequate coverage. A fundamental restructuring of healthcare delivery systems is crucial to achieving universal health coverage (UHC) in a cost-effective manner. This transformation necessitates a shift from the conventional model to an assurance-based approach underpinned by technology-driven processes.
The Escalating Cost Burden
Healthcare costs have been rising exponentially, exacerbated by factors such as aging populations, increasing prevalence of chronic diseases, and technological advancements in treatments. According to the World Health Organization, global healthcare spending is projected to surge by 6.3% annually, reaching $15 trillion by 2025. This trajectory is simply unsustainable, particularly for developing nations grappling with resource constraints.
Conventional healthcare models, typically involving fee-for-service payments, incentivize overutilization of services and contribute to wasteful spending. A study by the Organisation for Economic Co-operation and Development (OECD) estimates that approximately one-fifth of healthcare expenditure is consumed by inefficient spending and redundant interventions.
The Assurance-Based UHC Model
The World Health Organization (WHO) defines UHC as "ensuring that all people have access to needed health services without suffering financial hardship." While this is a noble goal, traditional UHC models often lack a focus on financial protection. People might have access to services, but out-of-pocket expenses can be a significant barrier, leading to delayed treatment, debt burdens, and even poverty.
A 2018 World Bank report emphasizes this point, stating that financial hardship due to healthcare costs pushes millions into poverty each year. This not only impacts individuals but also weakens healthcare systems as unpaid bills strain resources. Assurance-based UHC addresses this by offering financial safeguards, ensuring people can access needed care without fear of financial ruin.
The Biju Swasthya Kalyan Yojana (BSKY) Program: A Pioneering Initiative
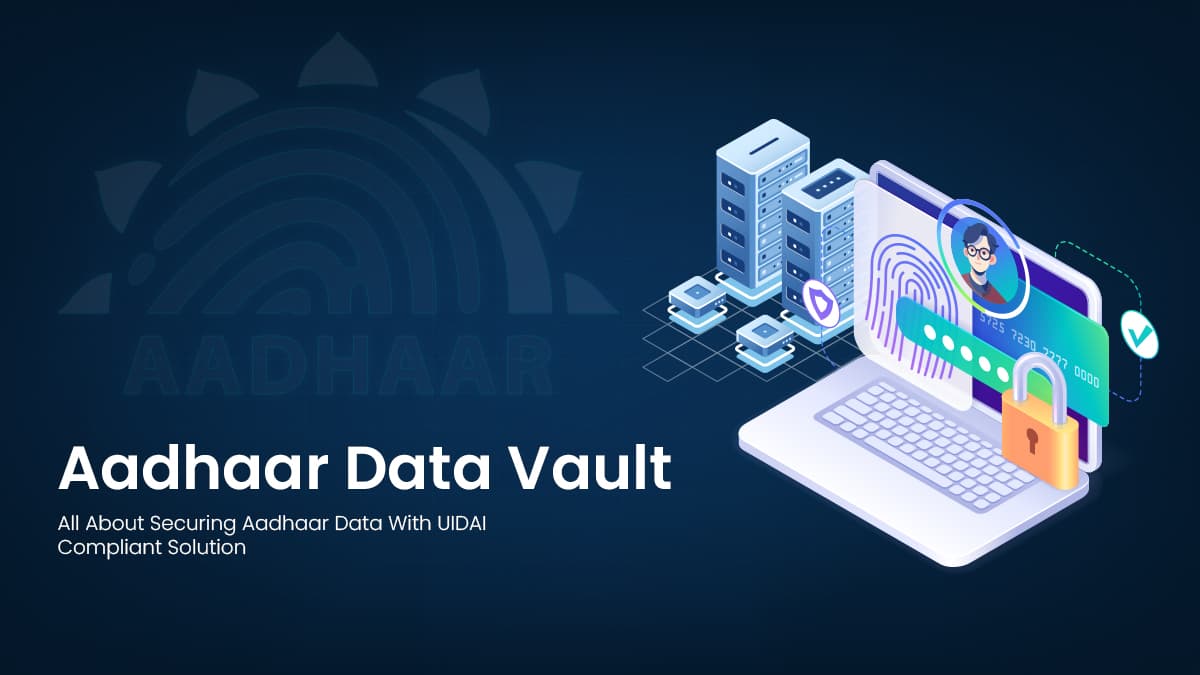
The Indian state of Odisha has emerged as a trailblazer in implementing an assurance-based UHC model through the Biju Swasthya Kalyan Yojana (BSKY) program. Launched in 2018, BSKY aims to provide comprehensive healthcare coverage to over 70% of Odisha's population, spanning both urban and rural areas.
The program's success hinges on a strategic partnership between the state government and a network of private healthcare providers. These providers are assigned a specific population base and receive capitated payments to manage the healthcare needs of their assigned beneficiaries effectively.
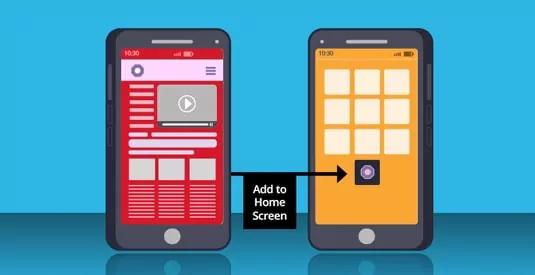
Technology plays a pivotal role in the BSKY program's implementation. A robust digital platform facilitates seamless data exchange, enabling real-time monitoring of health outcomes, service utilization, and costs. This data-driven approach empowers evidence-based decision-making, fosters transparency, and ensures accountability among stakeholders.
The impact of BSKY has been profoundly positive. A recent survey by the Odisha State Health Assurance Society revealed that 87% of beneficiaries reported improved access to healthcare services, while 92% expressed satisfaction with the quality of care received. Additionally, the program has contributed to a significant reduction in out-of-pocket expenditures, alleviating the financial burden on households.
Embracing the Assurance-Based UHC Paradigm
.jpg)
As nations grapple with the dual challenges of escalating healthcare costs and insufficient coverage, the assurance-based UHC model emerges as a compelling solution. By aligning incentives, fostering collaboration, and leveraging technology, this approach holds the promise of achieving universal health coverage while optimizing resource utilization.
The success of initiatives like the BSKY program in Odisha underscores the feasibility and efficacy of this transformative model. However, its widespread adoption requires a concerted effort from policymakers, healthcare providers, and stakeholders across the healthcare ecosystem.





































We will verify and publish your comment soon.