Global health systems are overwhelmed and understaffed. Hospitals have squeezed every possible efficiency out of healthcare workers, and doing administrative tasks takes up an alarmingly large percentage of providers' time compared to that spent treating patients. The use of artificial intelligence tools—such as voice-to-text transcriptions for prescriptions and chart notes, and automated staffing schedulers—is starting to reduce the administrative burden.
Automating insurance coverage verifications and low-risk prior authorizations could be the next major step for healthcare leaders trying to innovate their way through the industry's labour shortage. Insurance claims and prior authorizations often require healthcare workers to make phone calls, send emails and texts, and, in some cases, fax forms to insurance companies—and then wait for responses.
Healthcare leaders who want to make strides with AI need to get comfortable with moving more quickly than they're used to—and the strong, established boundaries between providers and insurance companies will have to be broken.
On average, a manual prior authorization takes an average of 21 minutes of staff time—and a single authorization can take up to 45 minutes, according to a 2021 report from the Council for Affordable Quality Healthcare (CAQH), a not-for-profit alliance of health plans, providers, government agencies, and standard-setting bodies. Automating prior authorizations would allow for much better use of highly trained healthcare professionals, making it a clear productivity win.
It's also a financial win. Insurance companies and other payers such as Medicare could save as much as $437 million per year by automating prior authorizations, according to the aforementioned CAQH report. The group estimates that the healthcare industry at large could reduce its administrative costs by $13.3 billion annually by fully employing automation.
Breaking Down Walls
_(1)_1730196035.jpeg)
One of the main obstacles to automating prior authorizations is the siloing of data between providers and insurance companies. The American Medical Association has been calling for a transition to automated and streamlined prior authorizations since at least 2018. Data uniformity and transparency from all levels of the healthcare system are key reforms principles prescribed in the organization's guiding documents. Still, prior authorization is one of the least active areas for implementing advanced computing by healthcare organizations, according to the CAQH.
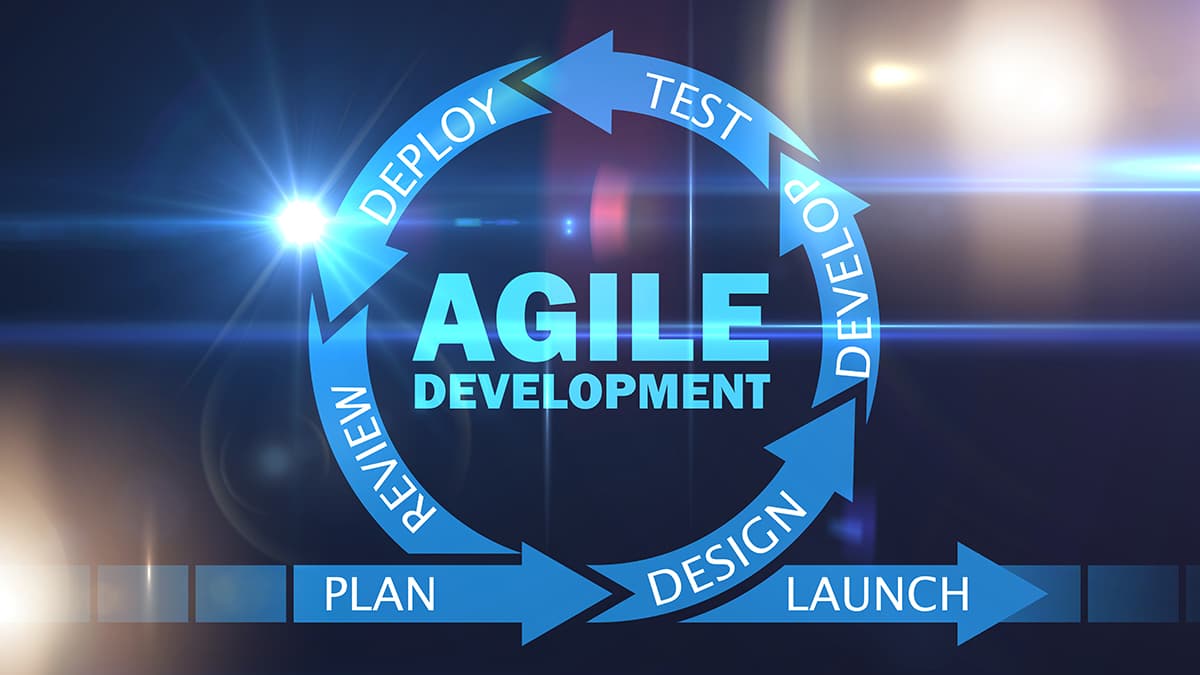
The healthcare industry moves very slowly, taking the same approach to IT as they do to new medical techniques and procedures: careful testing in a controlled environment, ensuring no harm, and adopting only if benefits outweigh costs. However, healthcare leaders pursuing AI advancement need to become comfortable with faster movement and breaking established provider-insurer boundaries.
Bringing in Top Talent
_1730196053.jpeg)
Competing for talent is an ongoing challenge for healthcare leaders trying to implement AI. Traditional healthcare companies have always struggled to compete for talent needed to make these leaps into advanced patient care. With large tech firms such as Google and AWS moving into the healthcare space, it's even harder for healthcare companies to secure full-time tech workers with advanced skills.
Technology has been changing exponentially while the talent market improves linearly, widening the gap daily. Healthcare companies need a robust talent model to effectively handle the future state. Using contingent talent teams with advanced computer modelling capabilities offers a cost-effective alternative to competing for scarce full-time tech workers, while maintaining nimbleness for innovation. Firms will also need access to operational workers—known as machine learning operations, or ML Ops—for day-to-day automation management.
Moving Forward With AI in Healthcare
_1730195968.jpeg)
Large healthcare firms are now using AI for customer service, billing, care management, and adjudicating claims. Some companies expect to automate 50% of their work over the coming years.
It's time for other forward-thinking health insurance companies to lead this charge. Information funnels through insurance companies as the payers, allowing them to build AI platforms conscious of claims information, clinical data, demographic information, and wearable data in what's called a data lake.
This deep flow of data enables automated minor prior authorization decisions and other processes. While adoption hesitancy may exist due to existing relationships, these barriers will fall as the system adapts to realize the substantial value for patients, benefiting all stakeholders equally.
At CSM, we work on emerging technologies like Robotic Process Automation (RPA), Machine Learning (ML), Generative AI and Industrial IoT to solve complex issues across domains like healthcare and citizen services.
Learn more about it here: www.csm.tech/service/emerging-technologies/
Want to start a project?
Get your Free ConsultationOur Recent Blog Posts

© 2025 CSM Tech Americas All Rights Reserved